20. Stroke– Update 13 Septr 2021
Here is a description of a carotid artery obstruction stroke:
It
was after eating lunch, early afternoon. While driving home, I ran a
red light. Then I stopped for a green light. When I got home I was
sitting in front of my computer, writing something.
I
remember the screen becoming a jumble of moving numbers and letters. I
then fell out of my chair, hitting my head hard on the concrete floor.
I tried, but could not get back on my feet.
My wife found
me lying on the floor and despite my protests called an ambulance She
was sure I had had a stroke, as my face was distorted, she said. They put in a stent. The
stent runs through my neck.
i’m not sure how high up.
Stroke, a Definition
Types of Stroke
Blood Clot due to Sluggish Circulation
Embolus from Heart
Brain hemorrhage due to high blood pressure and/or aneurysm
Brain Tumor Induced Stroke
Lacunar Strokes
Transient Ischemic Attack “TIA”
Stroke in Spinal Cord
Circulation to the Brain
Stroke Prevention Tests
Stroke Prevention Behaviors
What to do if stroke suspected
About Neuroimaging
Stroke, a Definition
Stroke is what the word suggests – sudden. The effects and affects of a stroke are long-lasting and that is what marks the stroke off from other sudden brain attacks like epilepsy, migraine or the closely related transient ischemic attack (TIA), all of which show rapid recovery. Now to real cases:
Types of Stroke
Blood Clot due to Sluggish Circulation: A 70 year/old, right-handed man takes an after-lunch nap. Daughter hears his snoring. When she wakes him, he is unable to speak or move right arm and leg.
Comment: Blood clot formed in an aging, cholesterol-narrowed, left-sided cerebral artery of dhis brain stops the artery's supply of oxygen and glucose, leading to damaged cerebral cortex motor neurons in rear left frontal lobe and including the Broca speech area and resulting in right-side body paralysis and loss of speech. Too high LDL-cholesterol from eating too many calories and too much animal fat in the setting of aging arteries with sleep-induced sluggish circulation brings it on. (A reason not to allow deep sleep!) Recovery depends on size of artery occluded and amount of brain tissue affected. A stroke should be hospitalized with neuroimaging (CT usually done first because more quickly available but MRI is more definitive) to localize blood clot or show hemorrhage. Also EKG and echocardiogram to check for heart disease source of cerebral artery embolus, and Doppler ultrasound test in the neck for narrowing/occlusion in the carotid arteries and branches. If no brain-bleeding detected or risked, initially, treat with aspirin or other anti-platelet drug. A rapid worsening with stupor to coma means high intracranial pressure usually from expanding hematoma (bleeding into the stroke area) and should get new MRI or CT and seen at once by neurosurgeon and, above all, should not get aspirin or other anti blood clotting drug.
Immediate treatment in Cerebral artery blood clot is thrombolysis, i.e., to inject an enzyme that dissolves the blood clot. It is either done into the arm vein (IV), which diffuses through the whole body, or by catheter threaded up into the local brain artery behind the clot. The IV injection is done by centers with less experience; it has an advantage of shortening the time to treatment, as it can be done by trained ambulance paramedic. But the injection through artery catheter gives best result (if done very soon after) and less risk to worsen stroke by hemorrhage; however, it is more complex and has its own serious complications. Decision to do thrombolysis or not is mostly out of a patient's control but if hemorrhage is suspected or risked, as in cases of high blood pressure, it should not be done.
Physiotherapy rehabilitation may restore lost function over several months. Low-dose aspirin or other anti-platelet aggregation and lower-cholesterol medication, after the stroke, is safe preventive as long as the stroke is not due to bleeding.
Immediate treatment in Cerebral artery blood clot is thrombolysis, i.e., to inject an enzyme that dissolves the blood clot. It is either done into the arm vein (IV), which diffuses through the whole body, or by catheter threaded up into the local brain artery behind the clot. The IV injection is done by centers with less experience; it has an advantage of shortening the time to treatment, as it can be done by trained ambulance paramedic. But the injection through artery catheter gives best result (if done very soon after) and less risk to worsen stroke by hemorrhage; however, it is more complex and has its own serious complications. Decision to do thrombolysis or not is mostly out of a patient's control but if hemorrhage is suspected or risked, as in cases of high blood pressure, it should not be done.
Physiotherapy rehabilitation may restore lost function over several months. Low-dose aspirin or other anti-platelet aggregation and lower-cholesterol medication, after the stroke, is safe preventive as long as the stroke is not due to bleeding.
Embolus from Heart: A 45-y/o woman arrives in a Tokyo hotel and is struck by a feeling of vertigo. Looking in mirror she sees a sagging left side of face and when she tries a toothy smile, her mouth pulls to right, showing a queer leer. She also notes weakness in her left extremities. Her speech is unaffected because she is right handed.
Comment: An embolic stroke from a mitral heart-valve blood clot that breaks off and travels up into the ascending aorta and enters its first major branch, the right side, and continues into its common carotid artery's internal branch to clog up an end branch of the middle cerebral artery and to cause a low-oxygen infarct to the motor cortex of rear right frontal lobe, most strongly to the area controlling the opposite left side lower facial muscles. The cause of such an embolus used to be rheumatic fever in childhood leading to a deformed, roughened mitral or aortic valve. More frequently now in 2021 such an embolus may be caused by the irregular-heartbeat atrial fibrillation or by a previous myocardial-infarction heart attack or an excessively floppy mitral valve (mitral valve prolapse) that some people are born with.
Prevention: Early stroke diagnosis by CT or MRI of brain to allow thrombolysis of the cerebral artery embolus-clot; also EKG and echocardiogram to check for heart atrial fibrillation (AF) and for a mitral or aortic heart valve lesion; and then if due to a valve lesion, it should have a carefully planned surgical repair or replacement followed by anticoagulant medicine. With atrial fibrillation or mild valve lesions, a life on anticoagulant is best.
Recovery from embolic stroke is good because the underlying cerebral artery is usually a small, healthy branch, and an alternative blood supply to the area prevents a complete infarct and allows time for dissolving the obstructing embolus with help of thrombolysis medicine and anticoagulant. But immediate hospitalization and expert care are needed.
Brain hemorrhage due to high blood pressure and/or aneurysm: A 36 y/o actress has headache and drops to floor in epileptic-type fit although no past history of epilepsy. She does not regain consciousness as expected with epileptic fit and an observer notes her eyeballs fixed in leftward gaze and right side of body as being limp due to paralysis.
An alternative: A 38 y/o woman on vacation in Hawaii at airport, waiting to board plane, experiences sudden pain behind right eye, slurring of speech and partial muscular weakness of left side but retains consciousness. Brought to ER, her BP is a very high 260/160 and her CT shows localized hemorrhage in right mid-brain.
Comment: The 2 cases represent stroke from hemorrhage in right side of brain through a tear in a cerebral artery caused by uncontrolled (and sometimes unrecognized) high Blood Pressure with or without a tiny aneurysm (ballooning out of weakened artery wall). The young age, here, of the strokes, suggests hemorrhage and also an oncoming stroke might have been suspected by the onset of a new migraine or behind-eye pain or a fit —-such premonitory symptoms known as TIA, or Transient Ischemic Attack. Also, sudden worsening of the stroke symptoms and stupor-coma suggest hemorrhage. The highest risk is in a patient taking Coumadin (Warfarin) pills or other anticoagulants - even aspirin - for heart problem or old thrombotic stroke. With any suspicion, get neuroimaging (CT, MRI) of brain. Un-ruptured cerebral aneurysm may today be treated without surgery. So the 2 main preventions are early discovery by MRA neuroimaging and then treatment, and control of hypertension.
Hemorrhagic strokes worsen because of brain swelling and blood clot enlargement with increased intracranial pressure; so they more often cause coma. But they are easiest to treat by a surgical opening of the bony cranium to evacuate clots, relieve the pressure, and stop hemorrhage. (Note the actress Patricia Neal; 41 years after her hemorrhagic stroke, living an active life and dying in her age 80's in Aug 2010.) A key to good result is rapid imaging diagnosis and access to top ICU stroke care.
Brain Tumor Induced Stroke: You sit in lecture at school listening to a 55-year-old professor speak about the Roman Empire. It is interesting but suddenly he is speaking unintelligibly. He appears normal and seems to have confidence in what he is saying, but has obviously lost his language.
Comment: A case of brain tumor compressing and finally cutting off small arteries that give vital supply of blood to brain cells of the dominant side of the professor's brain in his front temporal lobe area responsible for speech intelligibility (Wernicke's area), in which the stroked person loses ability to understand his speech (fluent aphasia) or writing (cause of acquired dyslexia), retains his ability to form the words and sentences but at first does not recognize his loss.
(Opposite of Broca’s aphasia described in the previous cases here.)
Lacunar Strokes are obstructions of small artery branches affecting the deeper cerebral (subcortical) white matter of brain just below cerebral cortex and leading to small brain cysts - lacunes. Single one may give no sign or symptom or may cause limited loss, but they usually increase in numbers and cause dementia. (Here is a description of discovery “she wasn’t making sense this morning I called an ambulance and they took her to the hospital”. This diagnosis has come to the fore since CT and MRI. It is almost always in an old age pre-dementia brain. Prevention: take lower-cholesterol pill (a statin like Lipitor) to keep LDL-cholesterol below 60 mg%, keep the resting BP and heart rate normal-low by beta blocker, ACE-I meds, and add-on, anti-hi-BP med; take low-dose aspirin daily and cut food intake but increase fluid intake by an extra liter water a day.
Lacunar Strokes are obstructions of small artery branches affecting the deeper cerebral (subcortical) white matter of brain just below cerebral cortex and leading to small brain cysts - lacunes. Single one may give no sign or symptom or may cause limited loss, but they usually increase in numbers and cause dementia. (Here is a description of discovery “she wasn’t making sense this morning I called an ambulance and they took her to the hospital”. This diagnosis has come to the fore since CT and MRI. It is almost always in an old age pre-dementia brain. Prevention: take lower-cholesterol pill (a statin like Lipitor) to keep LDL-cholesterol below 60 mg%, keep the resting BP and heart rate normal-low by beta blocker, ACE-I meds, and add-on, anti-hi-BP med; take low-dose aspirin daily and cut food intake but increase fluid intake by an extra liter water a day.
Transient Ischemic Attack “TIA”: An imminent stroke warning is important to recognize as it may occur and recur days to years before stroke, and recognizing a TIA allows treatment (replacement of narrowed artery segment or damaged heart valve, lowering high BP, removal of brain tumor; and check for brain aneurysm) to head off stroke. It shows as sudden, temporary weakness of arm or leg, loss of speech, temporary amnesia, temporary double vision or loss of vision in eye, or vertigo; or even a new migraine or severe headache. It is the recovery and repetitiveness of symptom that suggest a TIA rather than a stroke or seizure or migraine.
The onset of a repetitive new type of seizure, a psychic aura or first migraine in an older age person may also predict stroke.
The onset of a repetitive new type of seizure, a psychic aura or first migraine in an older age person may also predict stroke.
Stroke in Spinal Cord: a man suddenly falls down and cannot get up while keeping conscious, and his BP is only slightly high, and his heart rate OK. Examination reveals muscle weakness in both legs, with pins and needles or numb feelings in feet and loss or weakness of rectal and bladder sphincter. Initial MRI diagnosis is transverse myelitis (destructive lesion horizontally across spinal cord typical of virus infection of cord or a manifestation of multiple sclerosis). Only a day later, from repeat MRI on the worsening symptoms, is it discovered that the man had suffered a spinal cord stroke due to block in blood flow from the aorta into spinal arteries as part of progressing dissecting aneurysm obstruction of upper aorta. Other causes of such a stroke could be embolus from aorta to spinal artery, or severe local arteriosclerosis or malformation in arteries from birth. In any case, rapid diagnosis could rescue a potential victim from a life of paraplegia. (Loss of control of both legs)
Circulation to the Brain Although Brain is 2% of body, it gets 20% of the blood circulation. It needs high rate of oxygen and glucose delivery constantly and if blood flow to brain is stopped, one's consciousness is lost after only 15 seconds and each minute that passes without circulation does damage and by five minutes it is permanent. All strokes are the effect of cutting off blood to part of brain or spinal cord. And the anatomy of the artery circulation is useful to all readers and is rather easy to recall.
Circulation to the Brain Although Brain is 2% of body, it gets 20% of the blood circulation. It needs high rate of oxygen and glucose delivery constantly and if blood flow to brain is stopped, one's consciousness is lost after only 15 seconds and each minute that passes without circulation does damage and by five minutes it is permanent. All strokes are the effect of cutting off blood to part of brain or spinal cord. And the anatomy of the artery circulation is useful to all readers and is rather easy to recall.
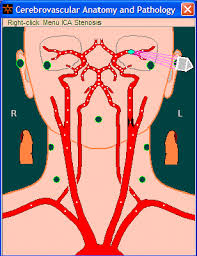
At bottom center of the above Figure you may just make out the top of the rounded arch of the ascending aorta, where oxygen-rich artery blood has just been pumped out of Heart's left ventricle, and, then, note, first, towards the Figure's right (the reader's left), the brachiocephalic artery coming off the aorta arch and almost immediately dividing into the right subclavian artery (to right shoulder) and right common carotid artery (up into right side of neck). And note the difference on the Figure's left (reader's right), where the left common carotid artery comes directly off the aorta arch almost immediately followed by the left subclavian artery. Also check the below (labeled) diagram as part of this reading now.
Now, consider timing: With each heartbeat, a pulse of blood is pumped into ascending aorta and the arch, and first the pulse goes up the right brachiocephalic and common carotid arteries, and, microsecond later, up the left common carotid artery.
Next, look at the paired right and left vertebral arteries which can be seen coming off the right and left subclavian arteries just as the subclavians make a small peak where the sides of neck become the shoulders. (Combined they form the shape of what looks to me like a condom sheathing an erect penis pointing upward through the neck.) Note how the vertebral arteries unite as they near the brain into a single artery, which is called "basilar artery" and supplies the rear brain.
Next return attention to the common carotid arteries and see that on each side they divide at the level of the lower face, and the inner branch is the internal carotid artery that supplies front of Brain and the outer branch is the external carotid artery that supplies the face and also interconnects with the branches of the internal carotid in the cranium, eyes and front of brain.
Then see, in the upper part behind the eye sockets, how the internal carotids in front and vertebrals-basilar in rear, which supply blood to front and back of Brain, unite in the Circle of Willis (the so called "circle" of arteries at base of brain, see below with labels). This uniting, or interconnecting, of the arteries is important in preventing strokes from occurring if either right or left vertebral or right or left carotid artery (or even both at once) become blocked, because the blood that would have been supplied to Brain by the blocked arter(y)(ies) can be siphoned into the brain by increasing the circulation of the remaining open major arteries.
Always when a stroke occurs, a Doppler ultrasound scan (a simple non-invasive test) on both sides of the neck should check for obstructions in the carotid arteries.
Now, consider timing: With each heartbeat, a pulse of blood is pumped into ascending aorta and the arch, and first the pulse goes up the right brachiocephalic and common carotid arteries, and, microsecond later, up the left common carotid artery.
Next, look at the paired right and left vertebral arteries which can be seen coming off the right and left subclavian arteries just as the subclavians make a small peak where the sides of neck become the shoulders. (Combined they form the shape of what looks to me like a condom sheathing an erect penis pointing upward through the neck.) Note how the vertebral arteries unite as they near the brain into a single artery, which is called "basilar artery" and supplies the rear brain.
Next return attention to the common carotid arteries and see that on each side they divide at the level of the lower face, and the inner branch is the internal carotid artery that supplies front of Brain and the outer branch is the external carotid artery that supplies the face and also interconnects with the branches of the internal carotid in the cranium, eyes and front of brain.
Then see, in the upper part behind the eye sockets, how the internal carotids in front and vertebrals-basilar in rear, which supply blood to front and back of Brain, unite in the Circle of Willis (the so called "circle" of arteries at base of brain, see below with labels). This uniting, or interconnecting, of the arteries is important in preventing strokes from occurring if either right or left vertebral or right or left carotid artery (or even both at once) become blocked, because the blood that would have been supplied to Brain by the blocked arter(y)(ies) can be siphoned into the brain by increasing the circulation of the remaining open major arteries.
Always when a stroke occurs, a Doppler ultrasound scan (a simple non-invasive test) on both sides of the neck should check for obstructions in the carotid arteries.
Note the labeling here and compare with the other, unlabeled Figure. Three major cerebral arteries come off the circle of Willis (More exactly, rather than a circle it is a pentagon) to supply parts of the brain and are important in most strokes. Forward (nearer top here) see the large middle cerebral arteries (the MCA, labeled on your left side). The MCA supplies much of the surface cerebral cortex and also because it is so wide-bore and is a direct continuation of the internal carotid artery it is the most common source of brain stroke by an embolus from the heart. Forward to it (Above it on both sides in the diagram) are the smaller, vertically upward directed paired parallel anterior cerebral arteries that supply the frontal area of brain. And in rear (Below in the Figure) you can see posterior cerebral arteries that supply the rear, right and left occipital lobes and the cerebellum. Also many smaller branches are indicated. Keep aware of the many connections between left and right side arteries protecting the brain tissue from artery blockage. But each small branch is an end-artery and, if it gets blocked, it gives a stroke that locates for the examining neurologist the place of the blood blockage. The MRI, by special MRA (magnetic resonance angiography or CT by CTA), can outline the whole brain artery circulation, relatively uninvasively, and should be done early after a stroke to locate potential areas of blockage or hemorrhage.
Stroke is due most commonly to thrombosis (blood clot block in artery) of aging artery after years of high LDL-choleesterol and can be prevented by keeping the LDL-cholesterol low. Less frequent and usually younger-age strokes are due to hemorrhage from hypertension or from blown-out aneurysms (small bulge in artery wall). Hemorrhage is most catastrophic because of brain swelling but also most accessible to treatment. Prevent by keeping Blood Pressure low normal and avoiding risk factors for hemorrhage like unnecessary aspirin or anticoagulants when one already has the risk from high blood pressure.
Least frequent are strokes due to embolus, which is a piece of blood clot broken off from a heart valve or heart wall or carotid artery wall. The embolus has the most sudden onset. A frequent cause of embolus is atrial fibrillation or mitral valve heart disease. Chronic anti-coagulant treatment or use of low dose aspirin in the absence of hypertension is a good preventive of an embolus.
Stroke is due most commonly to thrombosis (blood clot block in artery) of aging artery after years of high LDL-choleesterol and can be prevented by keeping the LDL-cholesterol low. Less frequent and usually younger-age strokes are due to hemorrhage from hypertension or from blown-out aneurysms (small bulge in artery wall). Hemorrhage is most catastrophic because of brain swelling but also most accessible to treatment. Prevent by keeping Blood Pressure low normal and avoiding risk factors for hemorrhage like unnecessary aspirin or anticoagulants when one already has the risk from high blood pressure.
Least frequent are strokes due to embolus, which is a piece of blood clot broken off from a heart valve or heart wall or carotid artery wall. The embolus has the most sudden onset. A frequent cause of embolus is atrial fibrillation or mitral valve heart disease. Chronic anti-coagulant treatment or use of low dose aspirin in the absence of hypertension is a good preventive of an embolus.
Stroke Prevention Tests
Do not disregard possible TIA symptom like dizziness, numbness, brief vision dimming or brief single-eye loss of vision or sudden headache.
With atrial fibrillation, get MRI (CT if MRI not available) of Brain and neck Doppler scan and echocardiogram, especially trans-esophageal, and EKG. If high risk or abnormal MRI or CT of brain, get an MRA or CTA (The A for angiogram). On a regular health exam, do not forget to remind your doctor to listen with stethoscope over both carotid arteries in neck: 25% carotid artery strokes may be predicted by loud murmur over the artery in the neck and can be prevented if discovered. The Doppler ultrasound test of carotid arteries in neck is the most important non-invasive check of carotid artery narrowing before it is clinically evident. Finally, but not leastly, brainwave EEG although it has low pick-up rate is a non-invasive, easy test for all types of brain pathology.
Do not disregard possible TIA symptom like dizziness, numbness, brief vision dimming or brief single-eye loss of vision or sudden headache.
With atrial fibrillation, get MRI (CT if MRI not available) of Brain and neck Doppler scan and echocardiogram, especially trans-esophageal, and EKG. If high risk or abnormal MRI or CT of brain, get an MRA or CTA (The A for angiogram). On a regular health exam, do not forget to remind your doctor to listen with stethoscope over both carotid arteries in neck: 25% carotid artery strokes may be predicted by loud murmur over the artery in the neck and can be prevented if discovered. The Doppler ultrasound test of carotid arteries in neck is the most important non-invasive check of carotid artery narrowing before it is clinically evident. Finally, but not leastly, brainwave EEG although it has low pick-up rate is a non-invasive, easy test for all types of brain pathology.
Stroke Prevention Behaviors
Keep sleep intervals short and light with low-lit, well vented bedroom and no inside-room space heater. If bowel movements are constipated, treat it with fruits and fluids. Above all, do not strain on toilet if constipated. If you must evacuate a constipated stool, use finger digital-assisted removal.
On waking from sleep or getting out of a hot (Temperature 41- to 42-degree or more C) bath, do not stand up quickly. Sit for a minute and move arms and legs, and take slow, deep breath and then slowly stand up.
Avoid over-exercise – anything that makes short of breath, gives rapid or bounding pulse, or dizziness.
Do not smoke; do not use cocaine or amphetamines or Ritalin; and limit alcohol to wine not more than a glass a day max with lots of water.
Drink water! Drink water! Drink water! (A liter of water on awakening morning dilutes blood, opens arteries, healthily elevates blood pressure and lowers risk of blood clot and LDL-cholesterol)
Do not take trip to far off places unless to see useful faces.
Check for and treat abnormal high blood pressure or heart rate. If atrial fibrillation (AF), take anti-stroke measures: low-dose aspirin or anticoagulant Coumadin if not hypertensive, lots of water daily and beta blocker med or digoxin to slow heart (Under your M.D.`s supervision, of course). If acute or recently new Atrial. Fib., try electrical conversion to normal rhythm after adequate anticoagulation and after esophageal echo test to rule out blood clot in left atrium of heart.
What to do if stroke suspected:
Call for ambulance saying it may be a stroke.
With unconscious patient, the observer should check carotid pulses in neck and respiration. A finding of no carotid pulse in a person just collapsed needs CPR (cardiopulmonary resuscitation). Feeling a good, regular, normal rate pulse with no respiration needs mouth-to-mouth breathing.
Assist stroke victim to lie on back with head on soft pillow, if not difficult to do, and, if possible, arms and legs elevated above heart. This position increases blood flow back to heart and ups cardiac output to brain.
If available, give 100% oxygen. (Ups oxygen saturation of blood plasma which may be crucial in limiting brain infarct)
If available, have assistant place ice collar (cubes of ice wrapped in towel or sheet) around neck and over skull. Low temperature in brain may limit brain damage and prevent sudden death; a reduction of 20 C (3.50 F) makes brain 30% more resistant to stroke from artery occlusion.
About Neuroimaging: First, CT and, second, MRI. The MRI is more accurate than CT. But CT is usually more quickly available.
Ultrasound is easy non invasive test, but to image the brain it is not revealing through an adult's skull. Ultrasound tests should include echocardiogram over the heart and behind by trans-esophageal and Doppler check of carotid arteries in neck.
The direct angiography of brain arteries from catheters stuck into femoral or carotid arteries are high risk and today in 2021 should mostly be replaced (except as part of thrombolysis for clot or for interventionist coil injection in hemorrhage) by MRA indirect angiography (CT angio may be done instead if MRA is not available).
END OF CHAPTER. To read next click 9.21 Mad Cow Disease - An Insider Story
About Neuroimaging: First, CT and, second, MRI. The MRI is more accurate than CT. But CT is usually more quickly available.
Ultrasound is easy non invasive test, but to image the brain it is not revealing through an adult's skull. Ultrasound tests should include echocardiogram over the heart and behind by trans-esophageal and Doppler check of carotid arteries in neck.
The direct angiography of brain arteries from catheters stuck into femoral or carotid arteries are high risk and today in 2021 should mostly be replaced (except as part of thrombolysis for clot or for interventionist coil injection in hemorrhage) by MRA indirect angiography (CT angio may be done instead if MRA is not available).
END OF CHAPTER. To read next click 9.21 Mad Cow Disease - An Insider Story

1 comment:
Nice Post
Get consultation for neurological disorders from one of the best neurologist in Delhi best neurologist in Delhi
Post a Comment