Physician's Notebooks 6 - http://physiciansnotebook.blogspot - see Homepage
This section also has Chapter 3 Heart Failure/Valves/Transplant scroll down
This section also has Chapter 3 Heart Failure/Valves/Transplant scroll down
Note: read carefully and supplement with Internet Wikipedia, and stop at short intervals to think about what you just read. And re-read if a subject is difficult!
.
.
2. Healthy Heart: Key to Healthy Life - Update 19 Aug. 2021
The following descending contents tells what is in Chap. 2 in order of the reading. Also use search & find. (For "cardiomyopathy" see Chapter 3.)
The following descending contents tells what is in Chap. 2 in order of the reading. Also use search & find. (For "cardiomyopathy" see Chapter 3.)
Intro
Illustration of Heart as a 4-chamber organ.
Description of Blood Flow
Muscles of the cardiovascular system
pulmonary circulation
The Heart Valves
The Heart Sounds
Mitral valve prolapse (MVP)
Intro: To live to age 100, your heart shall have to beat 4-billion times—-a lot of work for one muscle. And what a muscle! A heart contracts automatically, and cannot stop beating without hell breaking loose. Heart is getting exercised whether you jog or lie on a sofa or tell a lie. To keep beating healthily to age 100, it needs not to overwork; it needs to do what the body needs but no more. It is a machine with constantly moving parts; and like Grandfather Clock it has a set number of strokes, at end of which is Stop. And Heart cannot get regular repair. So conserve its function by striving for slow, resting heartbeat with help of beta blocker & ACE inhibitor medicine after age 50. Also, when you do not need to be active, rest; and sit, or lie down when you do not need to stand.
Illustration of Heart as a 4-chamber organ.
RA & LA are right & left atriums (alternative plural "atria"); RV & LV are right & left ventricles.
In the Systemic Veins (directed into right side of heart, cf. pulmonic veins directed into lungs), oxygen-poor blood flows back to Heart. The upper-body vein-blood flows down from Head assisted by gravity (in standing & sitting) and enters RA. The lower-body vein blood flows up to Heart into RA. In erect position the blood flow from lower veins is opposed by gravity so needs help by skeletal muscles that act as pump and the veins have internal valves that direct the blood flow towards Heart.
Description of Blood Flow: From the RA, oxygen-poor, dark blood flows through the tricuspid heart valve from RA to RV, is pumped out of RV through the pulmonic valve into the Pulmonary Artery into right and left in lungs, and continues branching into millions of smaller branches to the capillaries which bring blood to lung aeration sacs (alveoli) where red blood cells give up carbon dioxide (CO2) and take up oxygen (O2). The O2 gets attached to each hemoglobin molecule in the red blood cell.
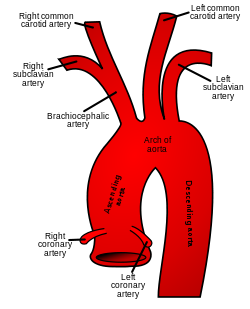
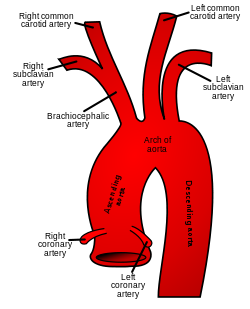
Then, the nearly 100% oxygen saturated hemoglobin-O2 bright red blood, after passing through the body tissue where the oxygen us used for metabolism and where CO2 is collected from the metabolism, flows back in pulmonary veins into the LA and, with help of the LA's pumping, flows through its mitral valve into the LV; and, then, the blood is pumped through the aortic valve into the ascending Aorta. Branches go up the ascending Aorta into the carotid arteries that give blood supply to the face and to Brain, and, just before that, into the subclavian arteries to the upper extremities (Note on right the origins of carotid and subclavian branches are united as the brachiocephalic, or innominate artery). And the rest of the heart's pumped arterial blood goes into the Aortic arch and down the descending Aorta into various artery branches that supply body tissues below the heart with the oxygen-rich blood.
Viewed from above head, the
Heart seems rotated counterclockwise about the
body's long axis so that the RV faces mostly front chest wall and toward
right side, and the LV faces partly the left front side of chest, and
the LA faces partly the back and is forward of the esophagus at
heart level. Orienting to the left breast nipple, the apex of a
normal-size heart is one rib gap below the nipple and slightly lateral
to it, and you may best feel your heart apex pulsation by fingertip between ribs there, leaning forward and to left after breathing out and holding breath. (If you do not feel it; that is still normal.) The systemic arteries carry oxygenated bright red blood from left side of heart and are thickly muscular. The systemic veins carry oxygen-poor, carbon-dioxide-rich, dark blood back to right side of heart and are thin-wall, elastic with few muscle fibers. Systemic artery branches come off the Aorta. The artery branches divide diminishing in size as they branch finally into arterioles and then capillaries, and each capillary, after its red blood cells unload its oxygen and nutrients and pick up carbon dioxide from cells, joining other distal capillaries to form a venule (tiny vein, like arteriole is to artery), which starts flow of blood back to the heart's RA.
Muscles of the cardiovascular system include muscle of the Heart and the muscle fibers in walls of arteries and veins; they are involuntary and unscripted in contrast to skeletal muscles, which are voluntary).
The voluntary skeletal muscles squeeze and relax on the thin-walled veins in the extremities to produce a muscle pump action on the vein. (But not on the arteries, which have their own muscle and whose thick walls resist the skeletal muscle pump)
About the pulmonary circulation; "Pulmonary" is not included when I use the word "systemic circulation", which refers to the circulation that starts on the left side of Heart and includes the LA, LV, Aorta and all its artery branches and capillaries and returning veins. The pulmonary circulation starts on the right side of the Heart and goes through the pulmonary arteries and branches, the lungs and pulmonary veins to, but not including, left side of Heart. From birth and during life, normally, the pulmonary circulation is low blood pressure compared to the systemic circulation. Medical conditions that increase resistance to flow in the pulmonary circulation - lung diseases especially bronchial asthma and air pollutant diseases like those that cigarette smokers get - cause pulmonary hypertension (PA BP > 50 mm Hg) and, eventually right-sided heart failure, whose symptoms are edema of legs with shortness of breath on normal exertion rather than the fatigue and fainting seen with left sided heart failure. Lung disease with right-sided heart failure is called COPD (Chronic Obstructive Pulmonary Disease) and today in 2021 it is frequent - most of the people in wheelchairs with oxygen cylinders - due to increasing air pollution. You can prevent COPD in yourself by not smoking or not being around smokers, by living in least air polluted areas (higher up better), by getting in habit of keeping mouth shut (not talking excessively), breathing through nose, and by otherwise being alert to the oxygen quality of your breathed air. (No indoor space heaters, but good ventilation at home, avoid car especially congested traffic)
About the pulmonary circulation; "Pulmonary" is not included when I use the word "systemic circulation", which refers to the circulation that starts on the left side of Heart and includes the LA, LV, Aorta and all its artery branches and capillaries and returning veins. The pulmonary circulation starts on the right side of the Heart and goes through the pulmonary arteries and branches, the lungs and pulmonary veins to, but not including, left side of Heart. From birth and during life, normally, the pulmonary circulation is low blood pressure compared to the systemic circulation. Medical conditions that increase resistance to flow in the pulmonary circulation - lung diseases especially bronchial asthma and air pollutant diseases like those that cigarette smokers get - cause pulmonary hypertension (PA BP > 50 mm Hg) and, eventually right-sided heart failure, whose symptoms are edema of legs with shortness of breath on normal exertion rather than the fatigue and fainting seen with left sided heart failure. Lung disease with right-sided heart failure is called COPD (Chronic Obstructive Pulmonary Disease) and today in 2021 it is frequent - most of the people in wheelchairs with oxygen cylinders - due to increasing air pollution. You can prevent COPD in yourself by not smoking or not being around smokers, by living in least air polluted areas (higher up better), by getting in habit of keeping mouth shut (not talking excessively), breathing through nose, and by otherwise being alert to the oxygen quality of your breathed air. (No indoor space heaters, but good ventilation at home, avoid car especially congested traffic)
The Heart Valves: In order as the blood circulation flows into right side of Heart: first, the tricuspid (3-flap) valve regulates blood flow between the RA and the RV and, although only rarely diseased, it is the most frequent site of infection in heroin drug-addicts from unclean IntraVenous (mainlining) injection; second, the pulmonic valve, between the RV and main pulmonary artery - least likely to need surgery; third, the mitral valve, between the LA and the LV - frequently weakened by old age heart failure and gives mitral regurgitation or gets narrowed after sore throat beta strep infection rheumatic fever into mitral stenosis which causes severe forward flow heart failure, congests the lungs and overloads the RV causing leg swelling -; and last, the aortic valve, between the LV and ascending aorta, frequently narrowed in old age, and especially with hypertension, and narrowed in aortic stenosis, and giving similar affects as mitral stenosis plus severely causing a damaging strain on the LV. A rarer disease of aortic valve is aortic regurgitation which mostly was caused by syphilis but now is caused by non-syphilis infection of the valve or very severe hypertension. Aortic regurgitation is well tolerated but eventually leads to overwork of the LV with wall thickening, left heart enlargement and terminal heart failure involving left and right sides of heart.
The Heart Sounds: The pulmonic and aortic valves pop open when the Heart's ventricles contract to squeeze out blood and slap shut when they relax; the tricuspid and mitral valves pop open when the Heart's ventricles relax and slap shut when they contract. These pop-open motions on ventricle contractions are part of the first heart sound. The slap-shot motion on heart relaxation makes the 2nd heart sound. (And see later chapter 6.15 for listening to the heart sounds w. Stethoscope.)
Valve damage may result in “insufficiency” (“regurgitation” mild very commonly seen in old age echocardiogram) in which a valve does not close enough and, oppositely, “stenosis” in which the valve sticks together, narrows and does not open well.
Mitral valve prolapse (MVP) shows on echocardiogram as a floppy ballooning of mitral valve back into the LA on valve closure. Twenty years ago it was a common, often mistaken diagnosis based on inaccurate examinations and tended to be over-treated and excessively worried over. Today, if a doctor says you have mitral valve prolapse, you should make sure the diagnosis is based on an echocardiogram. An MVP in the absence of other heart abnormality is now considered a benign variant that needs no treatment.
Many heart valve disease patients today are getting heart valve repair or replacement. The decision for surgery and type of valve should be decided at top centers and, unless done for emergency heart failure, firmed by 2nd and even 3rd cardiology opinion. Today, biologic heart valves from pigs, cows or horses are usually preferred for persons over 65 because of less need for anticoagulant-for-life treatment. Mechanical heart valves tend to be preferred for younger patients because of their permanency; biologic valves deteriorate at high rate after 10 years and will need to be replaced. But exact decision should be on a case basis by top heart surgical team firmed by independent cardiology opinion.s
END CHAPTER 2
Chapter 3. Heart Failure (HF)/Transplant
Descending contents show what's in the chapter in order of reading.
Descending contents show what's in the chapter in order of reading.
What is it?
Cardiomyopathy
Right and Left Side Failure
Signs and Symptoms of HF
Tests for Heart Failure
Preventives of Heart Failure
Treatments of heart failure
Heart Transplant
What is it? Failure of Heart to pump blood around body. Its mechanisms are: Pump failure due to heart muscle being locally damaged (myocardial infarction) or generally diseased (myocarditis or cardiomyopathy); too high resistance to forward flow failure (Resistance in arteries from hypertension causing thickened left-sided heart failure, or pulmonary artery hypertension from chronic lung disease causing right-sided heart failure); obstruction to forward flow failure due to valve malfunction as in aortic stenosis of old age causing failure of forward flow and backing up blood in the heart chambers behind; or back flow failure (shunt) from “hole” in heart between chambers (septal defect) or abnormal flow between pulmonary artery and aorta (patent ductus arteriosus), or because damaged valve cannot close completely due to valve insufficiency (regurgitation).
Cardiomyopathy is a heart failure due to weak malfunctioning heart muscle. It is usually left ventricular of 2 types: widespread myocardial ischemia that damages wide area of muscle or non-ischemic where chronic poorly or untreated hypertension causes a thickened left ventricular wall that has lost its give. Other divisions are based on shape. It is an end stage heart failure and usual cause for heart transplantation.
Cardiomyopathy is a heart failure due to weak malfunctioning heart muscle. It is usually left ventricular of 2 types: widespread myocardial ischemia that damages wide area of muscle or non-ischemic where chronic poorly or untreated hypertension causes a thickened left ventricular wall that has lost its give. Other divisions are based on shape. It is an end stage heart failure and usual cause for heart transplantation.
Right and Left Side Failure: In causes of Heart Failure, the heart’s Right Ventricle fails to pump enough blood to lungs (right side failure) or the Left Ventricle
Signs and Symptoms of HF
1) Fatigue (More with left-side failure of forward flow): Earliest and least sensitive or least specific symptom of HF, it is the tendency to fade quickly, a decreased capacity for work. Most typical in gradual HF, it is a ‘creep up’ symptom usually realized only in retrospect. Rapid heart rate with mild exertion should be found associated with the fatigue of HF.
2) Rapid Resting Heart Rate: When Heart fails, the 1st compensation is to increase the heartbeat per minute to make up for smaller volume of blood being delivered into aorta with each beat. Increased HR at rest is a highly sensitive sign of early failure. But if there is a heart block - as can be seen on EKG - a fixed, very slow heart rate (30 bpm) may be the cause of the heart failure. Also patients taking beta blocker or calcium channel blocker medication may have slowed heart rates despite going into HF.
3) Shortness of Breath (SOB, or Dyspnea) brings patients to a doctor sooner but can creep up or have other cause (nervous hyperventilation, lung disease, anemia). It is related to exertion and position. Anyone gets SOB climbing too many steps too fast; in heart failure it is a worsening over weeks to months. At rest in HF, a high respiratory rate is found with patient in bed with shoulder flat on mattress and progressively improves as one puts pillows under shoulder and elevates upper chest.
A striking SOB, seen with high-BP heart failure is paroxysmal nocturnal dyspnea. Suddenly, in middle of cold winter night, victim wakes gasping and seeks relief by rushing to window, flinging it open and breathing cold air. Actually, the relief is from the erect position. The worst SOB, pulmonary edema, is end stage HF. Patient breathes rapidly and shallowly, blood-tinged foam comes from throat, skin color is florid to bluish about lips, and death comes soon if no treatment.
A striking SOB, seen with high-BP heart failure is paroxysmal nocturnal dyspnea. Suddenly, in middle of cold winter night, victim wakes gasping and seeks relief by rushing to window, flinging it open and breathing cold air. Actually, the relief is from the erect position. The worst SOB, pulmonary edema, is end stage HF. Patient breathes rapidly and shallowly, blood-tinged foam comes from throat, skin color is florid to bluish about lips, and death comes soon if no treatment.
4) Distension of Veins of Hand and in Neck is best seen seated. Start by allowing your dominant hand to dangle alongside body. Then, observe the back of your hand's blue veins that are normally distended with blood in that position, while gradually lifting forearm with back of hand facing you and arm not crooked, and observe distension of veins. As your hand lifts to above level of heart, the veins should normally empty and become less detectable. With heart failure the veins remain distended with hand held at or above heart level. (How high above heart level the veins remain distended depends on severity of the HF.) This test depends much on size of veins of hand. In woman or child and fat person they are not well seen. Also jugular vein on side of neck is useful to observe. Position should be with shoulder and head elevated 300 to 450 above horizontal. If the neck veins remain distended compared to flat in bed position where normally distended, it means HF. Distention of veins develops late in heart failure especially with right side failure and is a very bad sign.
5) Ankles Swelling: Early symptom of HF involves feet and ankles on both sides equally, worst at end of day, and least on waking in bed. Except in late case, it does not involve hands or eyes. It is an early HF sign that may first be evident several hours into long jet flight in economy class seat.
6) Gallop rhythm on heart auscultation is a sign only a doctor with stethoscope can detect but very serious.
6) Gallop rhythm on heart auscultation is a sign only a doctor with stethoscope can detect but very serious.
Tests for Heart Failure:
Earliest blood test is the BNP (blood natriuretic protein test), which rises before any sign or symptom.(But very non-specific and seen with apparently normal heart.) Most accurate test is the Ejection Fraction (EF by echocardiogram) of heart left ventricle. The EF should be more than 0.45 (>45%) in normal. But normal EF number may be seen with early HF if decreased from previous high normal. Also uncomplicated right sided heart failure at start gives normal EF. The chest X-ray shows HF from pattern of distended blood vessels in lung. The EKG often shows a right ventricular strain pattern.
Earliest blood test is the BNP (blood natriuretic protein test), which rises before any sign or symptom.(But very non-specific and seen with apparently normal heart.) Most accurate test is the Ejection Fraction (EF by echocardiogram) of heart left ventricle. The EF should be more than 0.45 (>45%) in normal. But normal EF number may be seen with early HF if decreased from previous high normal. Also uncomplicated right sided heart failure at start gives normal EF. The chest X-ray shows HF from pattern of distended blood vessels in lung. The EKG often shows a right ventricular strain pattern.
In detecting HF, let’s have fun with a Yes/No flow-sheet. It starts with checking resting heartbeat rate per minute. (After a 15-min repose, take your pulse or listen to heart) Then the Yes/No:
Is your resting heartbeat abnormally fast?
Yes. .
↓
Have you sign or symptom of HF?
↓ ↓
Yes No.
You have HF. .
Get blood test BNP, Echo, chest x-ray & EKG .
The above is useful because by focusing on the easily obtained heartbeat rate it directs you rapidly to diagnosis.
Preventives of Heart Failure: Weight you carry around adds to burden on heart work, especially with heart failure. An inadvertent weight is your clothing. The lighter weight your clothes are, the less work for your heart. Also your body weight. Fluid with salt intake, when excessive, overloads your blood circulation and over-stresses heart. If you show HF or risk factor, avoid excess (But still, enjoy your food at reasonable levels salt.) fluid with salt and excess alcohol. (Beer binge the worst.)
Most important: keep your resting heart rate (pulse rate on awakening) between 55 and 70 bpm (beats per min.); it may need a beta-blocker medication and an ACE-inhibitor under your treating physician`s supervision. (I`ve been on both medications for 10 years and no problems and morning bpm always around 55 to 65.)
Keep LDL cholesterol below 60 mg%, keep BP around or below 120/60-70 and keep well oxygenated (Avoid carbon monoxide/low oxygen breathing space like inside driving car, sudden high altitude; learn good breathing technique and, if at risk for HF, have oxygen canister with mask or nasal cannula at home and workplace.)
The ideal Body Mass Index against HF should be BMI 18 to 20 especially by old age so keep low healthy weight.
Treatments of heart failure after preventives start with diuretics like chlorthiazide that reduce salt and fluid load by peeing it out. Next step is heart muscle strengthener like Digoxin but it needs careful physician monitoring.
Attention to heart rhythm very important. If you have the common atrial fibrillation or flutter, then a chemical or electrical conversion to sinus rhythm may relieve the heart failure. If not possible, a beta-blocker slowing of resting heart rate will add years to life.
A special dangerous risk is A-V heart block, frequent in old age due to the aging's wear and tear, which gives a fixed very slow heart rate c.30 bpm. A pacemaker solves the problem and no need for medication.
Heart Transplant is final option. You got to be in severe heart failure where all medical approaches have been tried and failed, you should be younger than age 70 and without chronic infections or cancers; in other words a good life expectancy if you had a good heart. Then, you need to have enough money - $100,000+ (or if insurance will cover).
Find a best place and put yourself into the hands of top team. Expect a risk of 10% of either dying on operating table or suffering stroke or other bad complication. Also expect a wait for a matching donor. If among the lucky 9 of 10 who get through the surgery intact, the latest results show good quality of life survival curve of 82%, 75%, 69% at 1, 2, and 5 years (totals include those who die during surgery); a 10-year survival of 50%, and 20-year survival of 20%.
Most important: keep your resting heart rate (pulse rate on awakening) between 55 and 70 bpm (beats per min.); it may need a beta-blocker medication and an ACE-inhibitor under your treating physician`s supervision. (I`ve been on both medications for 10 years and no problems and morning bpm always around 55 to 65.)
Keep LDL cholesterol below 60 mg%, keep BP around or below 120/60-70 and keep well oxygenated (Avoid carbon monoxide/low oxygen breathing space like inside driving car, sudden high altitude; learn good breathing technique and, if at risk for HF, have oxygen canister with mask or nasal cannula at home and workplace.)
The ideal Body Mass Index against HF should be BMI 18 to 20 especially by old age so keep low healthy weight.
Treatments of heart failure after preventives start with diuretics like chlorthiazide that reduce salt and fluid load by peeing it out. Next step is heart muscle strengthener like Digoxin but it needs careful physician monitoring.
Attention to heart rhythm very important. If you have the common atrial fibrillation or flutter, then a chemical or electrical conversion to sinus rhythm may relieve the heart failure. If not possible, a beta-blocker slowing of resting heart rate will add years to life.
A special dangerous risk is A-V heart block, frequent in old age due to the aging's wear and tear, which gives a fixed very slow heart rate c.30 bpm. A pacemaker solves the problem and no need for medication.
Heart Transplant is final option. You got to be in severe heart failure where all medical approaches have been tried and failed, you should be younger than age 70 and without chronic infections or cancers; in other words a good life expectancy if you had a good heart. Then, you need to have enough money - $100,000+ (or if insurance will cover).
Find a best place and put yourself into the hands of top team. Expect a risk of 10% of either dying on operating table or suffering stroke or other bad complication. Also expect a wait for a matching donor. If among the lucky 9 of 10 who get through the surgery intact, the latest results show good quality of life survival curve of 82%, 75%, 69% at 1, 2, and 5 years (totals include those who die during surgery); a 10-year survival of 50%, and 20-year survival of 20%.
End of Chapter. To read next, now, click 6.4 Nerves and Neurotransmitters in the Heart

No comments:
Post a Comment